Learning from the dead to help the living
The lungs are the primary, but not the only target of Covid-19. Early in the pandemic, Basel researchers were among the first to venture to perform autopsies on deceased Covid-19 patients, making important contributions to our understanding of the new infectious disease. Professor Alexandar Tzankov of the University of Basel is leading a research project highlighting the effects of the virus on the body’s tissues and organs.
18 March 2021
When a mysterious respiratory illness began to spread in late 2019, a particular medical specialty that had long been declared dead suddenly reclaimed the limelight: the autopsy. Clinical autopsies are conducted by pathologists, medical specialists concerned with abnormal morphological changes in the body and its tissues aiming to diagnose disease and gain understanding of their origins. Alexandar Tzankov became fascinated with them during his undergraduate studies when he read the seminal textbook Robbins Pathologic Basis of Disease. Looking back, he says of his decision: “I wanted the body’s tissues to speak to me.”
Tzankov’s team and their colleagues in Basel-Landschaft and Hamburg were among the first to perform postmortems on deceased Covid-19 patients on a larger scale. “Many of these autopsies are taking place all over the world now – the field has gotten a second wind,” says the pathologist. He leads a project that is studying the effects of the Sars-CoV-2 virus on different tissues in the body. They have already published several findings from their research, supported by the Botnar Research Centre for Child Health (BRCCH) with CHF 1.3 million, in a series of papers.
Spotlight on finely branching blood vessels
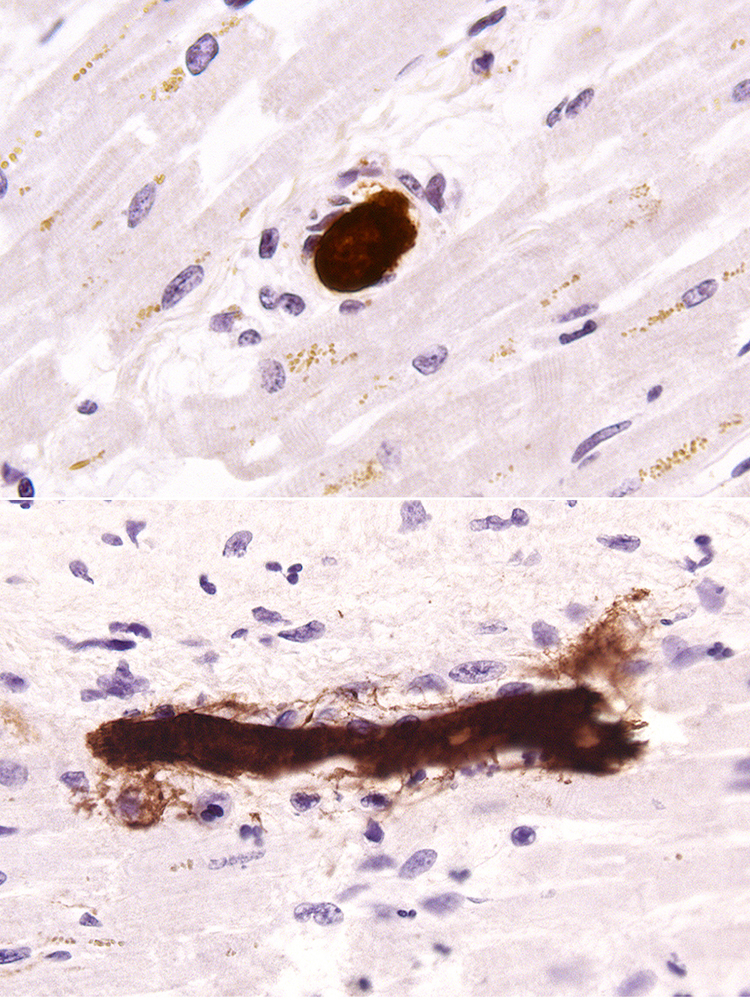
The first analyses of the lung tissue of deceased Covid-19 patients already revealed surprises. “We did see diffuse damage to the pulmonary alveoli, but nowhere near as much as in other deadly viral respiratory diseases,” says Tzankov, who has to take a short break from the video call to see to a tissue sample. Tissue waits for no man.
The bigger problem with Covid-19, reported Tzankov and other pathologists in the New England Journal of Medicine last summer, is micro-clots in the finely branching blood vessels of the pulmonary alveoli. The new coronavirus-induced disease causes ten times more of these microthrombi than what is observable in influenza virus-induced lung injury.
The organism also seems unable to replace the blocked and non-functional blood vessels. “Although a molecular cascade is triggered to form new vessels, it fails and doesn’t lead to functioning micro-circulation,” Tzankov says in summary. The consequence is inadequate gas exchange at the lung membrane because oxygen transporation is tightly related to functioning micro-circulation.
Because transport of CO2 is less affected, patients display a phenomenon called “happy hypoxia.” An excess of CO2 in the blood normally causes feelings of suffocation. But since the CO2 is transported away relatively well, even though little oxygen can be transported in, patients seem not to notice that they are suffocating.
No direct damage to the brain
The problem goes far beyond the lungs: the virus can be detected in small quantities in practically every tissue of the body and can disrupt, along the body response to the infection, the local micro-circulation of the blood. For example, Tzankov believes that aphasias, vestibular complaints, and chronic fatigue – collectively called post-Covid-19 syndrome, which persists long after the acute infection – are likewise attributable to problems with micro-circulation and not to damage to nerve cells caused by the virus, as initially assumed.
The insight that the virus wreaks its greatest havoc on the blood vessels is among the most significant findings to be gained through pathology during the pandemic. It highlighted that the condition of the vascular system can determine how tolerant the human body is of Sars-CoV-2 and how an infection is proceeding. And it pointed to promising approaches like the use of anticoagulants to ward off fatal consequences of infection in at least some patients.
“In this exceptional global situation, pathology was able to show that we can learn things from the dead that are directly applicable to the living,” says Tzankov. He and his team continue to follow the tracks of the virus in the body’s various tissues. Thanks to the funding provided by the BRCCH, they have new resources and collaborations with a network of national and international research groups at their disposal.
Further information
Prof. Dr. Alexandar Tzankov, University of Basel, University Hospital Basel, phone +41 61 265 3229, email: alexandar.tzankov@usb.ch