Keeping metastases in check.
Text: Andreas Lorenz-Meyer
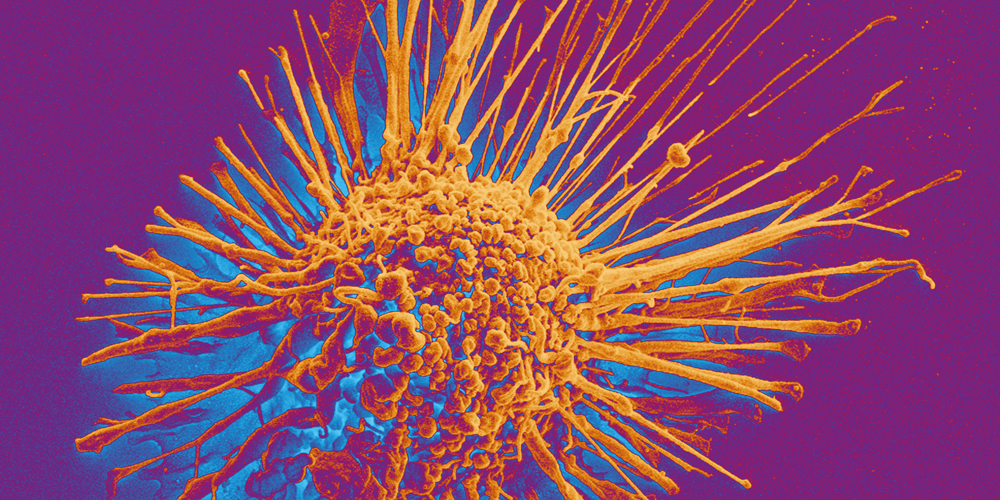
When cancer metastasizes, the prognosis gets worse. Basic research reveals ways to prevent metastasis.
Ovarian cancer can grow for a long time without causing any pain because it has plenty of space to proliferate inside the pelvic and abdominal cavities. This allows it to spread undetected. Often, it is only discovered at a very late stage when the cancer has already begun to metastasize. That is why ovarian cancer is considered the most lethal form of cancer among women.
With ovarian cancer, metastases spread relatively quickly, but are generally confined to the abdominal cavity. In addition to affecting the fallopian tubes, secondary cancers may also develop on the peritoneum, the lymph nodes and the digestive tract.
Cells in limbo
For tumors to metastasize in the first place, their cells must be able to change and adapt. As they make their way through the abdomen, the cells pass through the bloodstream and lymph system – completely new environments from that of the ovarian tissue where they originated. This ability of cancer cells to adapt to changes is known in professional circles as “cell plasticity”. It is based on a specialized process, a type of metamorphosis in which the cells undergo changes to their form and properties. Specialists refer to this metamorphosis as “epithelial-mesenchymal transition” (EMT), and in other contexts, it can be a good thing: The same process is required for embryonal development and wound healing. But it also allows cancer cells to detach from the primary tumor and spread.
Some cells remain in an intermediate state of metamorphosis. “These cancer cells are the most versatile; they are the engine of the metastatic process,” says Francis Jacob, who studies ovarian cancer at the Department of Biomedicine.
Jacob is searching for methods to inhibit tumor cell plasticity. His approach involves specialized molecules that are found in large numbers on the surfaces of the body's cells. “Glycolipids”, as these molecules are called, consist of a sugar group and a fat group. They are one of the basic components of every cell membrane in our body: “For example, they determine your blood type. Some glycolipids are present on stem cells, and they are part of what gives these cells their special properties,” explains Jacob.
Yet Jacob’s main focus is on a subgroup of glycolipids that are highly prevalent on metastasizing ovarian cancer cells and play a key role in their metamorphosis: They help the tumor cells achieve cell plasticity and transfer information between these cells. They serve as an intercellular communication system: One cancer cell uses specialized glycolipids to send a signal to neighboring cells, letting them know, for instance, how to adapt to conditions in the bloodstream.
But how can we suppress this communication between cancer cells? The solution could lie in the glycolipid repertoire, or the aggregate of the different types of glycolipids found on the surface of a cell. “It's like a fingerprint that allows cells to recognize and communicate with one another. We want to decode this fingerprint so that we can better understand the communication between cancer cells and develop more targeted cancer treatment options,” explains Jacob.
Until now, the approach to treating ovarian cancer focused on certain proteins that, while prevalent on the surface of tumor cells, can also be found on the membranes of healthy cells. According to Jacob, that means treatments are not as specific as they could be.
Forcing cells to reverse course
Jacob thinks it is possible to develop two new therapeutic approaches. The first involves attacking the glycolipid profiles that are typical of cancer cells – not unlike conventional cancer therapies that target a particular protein that is more or less specific to cancer cells. The second involves forcing metastatic tumor cells to reverse their metamorphosis and return to their original state. This could slow down or even stop metastasis in its tracks.
Evidence is already beginning to emerge in the search for an agent to reverse the metamorphosis of cancer cells: For instance, the toxin produced by the bacterium that causes cholera can reverse EMT and, in so doing, suppress metastasis. This discovery was originally made by US-based scientist Robert A. Weinberg. Francis Jacob and his team have taken the next step: “We’ve shown that certain glycolipids play key roles in this reversal process – without them it wouldn't work very well.”
Now, the research team simply has to find an agent less dangerous than the cholera toxin that also binds the right kinds of glycolipids. This would interrupt the communication system between the cancer cells. Then they would no longer be as flexible in adjusting to new environments as they spread – an important step in the battle against metastases.
More articles in this issue of UNI NOVA (May 2023).