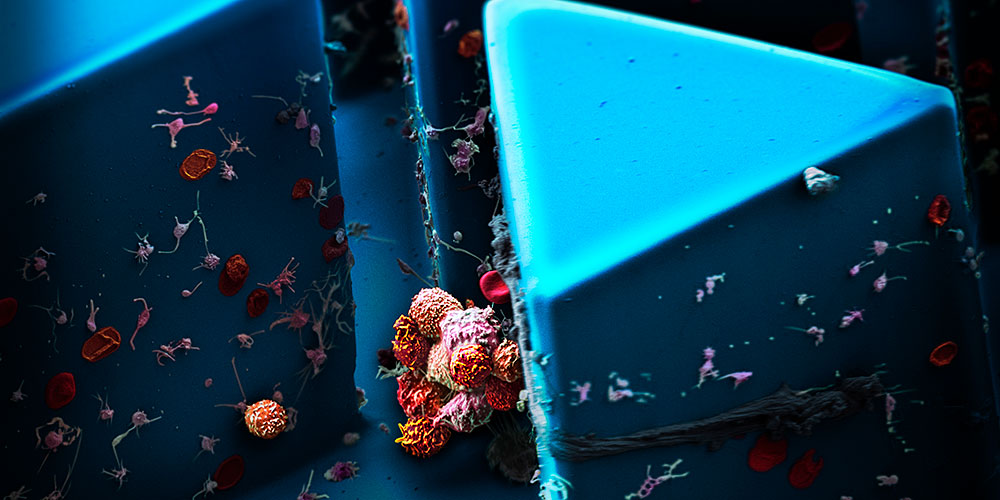
Tracking metastasis.
Text: Yvonne Vahlensieck
When cancer cells break away from tumors and enter the bloodstream, they can develop into metastases. Researchers at the Department of Biomedicine are investigating precisely how this process works – and developing new concepts for cancer treatment.
Oncological medicine has come a long way in recent decades. Many cancer types can now be effectively treated, provided the tumor is diagnosed early. Once the tumor spreads, however, chances of survival plummet: Around 90% of cancerrelated deaths are caused by metastases, which do not respond to conventional treatment methods.
Accordingly, researchers are increasingly focusing their attention on ways to combat metastasis. The fundamental mechanism behind metastasis is clear enough: Cancerous cells break away from the primary tumor and are carried by the bloodstream or lymphatic system to other tissues such as bone, lungs or liver, where they grow into metastases. However, the exact processes at work are still largely unknown. This is why a research group at the Department of Biomedicine has set itself the goal of finding out more about the cells circulating in the bloodstream that give rise to metastases: “If we can find a way to prevent these cells from forming or to destroy them, then we can stop the cancer from spreading and increase life expectancy,” says Professor Nicola Aceto, the oncologist in charge of the Cancer Metastasis Laboratory.
Cancer cells on the move
The first step in studying these cells, known as circulating tumor cells, is to isolate them from the blood of cancer patients. This is easier said than done: “A test tube of blood contains some 50 billion blood cells, and just one to ten circulating tumor cells,” Aceto explains. However, the tumor cells are a few thousandths of a millimeter larger than blood cells. This size difference gives the researchers a handy way to capture tumor cells: They direct the sample
through a maze of increasingly narrow channels onto a microchip. Blood cells pass through the channels unhindered, while the slightly larger tumor cells are caught as if in a trap.
The circulating tumor cells isolated in this way can then be examined more closely using molecular biology techniques. Aceto has also succeeded in keeping the cells alive and cultivating them in petri dishes, although to achieve this the team had to delve deep into their bag of tricks: The process requires specially coated containers, a particular nutrient solution and a low-oxygen environment. These cell cultures are not just used for experiments – Aceto has hopes for clinical applications, too: “We can isolate the circulating tumor cells in a patient, replicate them and then use the cultures to test a variety of different drugs.” In future, this procedure could help oncologists select the most effective treatment, particularly for patients with advanced metastases.
Studying the cells captured by the microchips has yielded numerous new insights over the last few years. For example, mouse models revealed that tumor cells only circulate in the blood for around ten minutes before disappearing again. “We believe that cells are constantly breaking away from the tumor, but most of them never metastasize, as they quickly die or are eliminated by the immune system,” Aceto explains. Only a tiny fraction of them appear to succeed in migrating to other sites and forming metastases.
Dangerous clusters
Another key finding was that circulating tumor cells do not always travel alone: They can form clusters of between 2 and 50 cells. These clusters play a key role in the emergence of metastases: In mouse models, circulating tumor cell clusters were found to be 20 to 50 times more likely to metastasize than individual cells. Moreover, in breast cancer patients the presence of these clusters in the bloodstream correlates with low life expectancy. A possible explanation ventured by Aceto is that the clusters are more likely than individual cells to be caught in the blood vessels of organs, allowing them to migrate into the surrounding tissue.
Close examination revealed that the clusters differ from lone circulating tumor cells in other ways, too: For instance, they produce a protein that helps hold the cluster together. Cluster cells also exhibited genetic alterations that activate certain subgroups of genes. This gives the cells properties similar to embryonic stem cells, which are able to multiply indefinitely. This could also be a significant factor in the process of metastasis.
With this in mind, Aceto is searching for substances able to break down the bonds that hold the clusters together, thereby inhibiting their metastatic potential. He has already found at least one promising candidate: By screening drugs that have already been approved, he came across a compound used to treat cardiac arrhythmia that can break up the cell clusters – at least in mouse models. What is more, treating mice with this substance did in fact lead to a reduction in metastases. Aceto is now testing the drug on breast cancer patients in collaboration with clinical oncologists at University Hospital Basel. “For now, however, the goal of the pilot study is simply to show that the concept works in principle,” says Aceto, adding that clinical trials and a potential treatment remain a long way off.
In the meantime, Aceto’s research group is also working on another unresolved aspect of metastasis – the question of why cells break away from the primary tumor in the first place: “A tumor is made up of billions of cells, and most of them remain where they are. Only a very small number leave the tumor.” This is another area in which Aceto sees great potential for future treatments: If cells can be prevented from leaving the tumor, then metastasis cannot occur.
More articles in the current issue of UNI NOVA.