Cancer: More targeted use of immunotherapy
Doctors are increasingly fighting cancer by stimulating patients’ immune systems. Researchers have now discovered a method for predicting the likelihood of treatment success, as reported by researchers from the University and the University Hospital Basel in the journal Nature Medicine.
12 June 2018
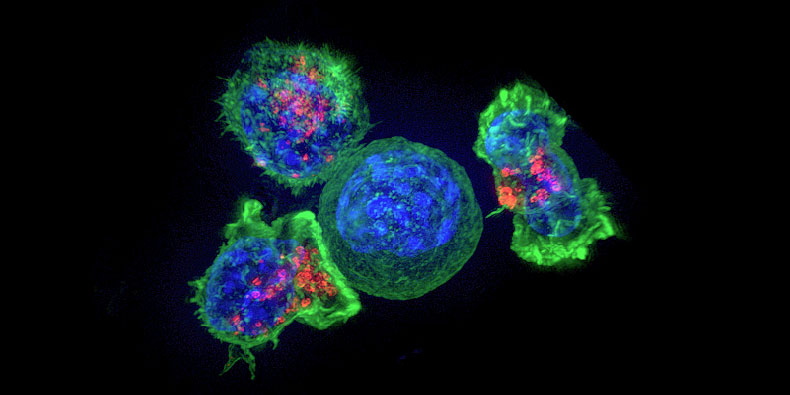
Immunotherapy changes a patient’s immune system to allow it to attack cancer cells and either destroy them or at least keep them from growing. But the therapy only works for a minority of patients. Researchers supported by the Swiss National Science Foundation (SNSF) have now discovered how to better predict who will respond to the therapy and who will not.
Unmasking tumors
The key is a protein known as PD-1, which sits on the surface of human immune cells. Until recently, PD-1 was regarded as their Achilles heel because cancer cells attach to the protein, thereby protecting themselves from immune system attack. “It’s as though the tumor were wearing camouflage,” says project lead Alfred Zippelius, Professor of Translational Oncology at the University of Basel and Deputy Head of Medical Oncology at University Hospital Basel. Immunotherapy blocks the attachment site so the immune cells can “see” the cancer again.
An international research group led by Zippelius has now shown that immune cells with the most PD-1 are best able to detect tumors. In addition, these PD-1–rich cells secrete a signaling compound that attracts additional immune cells to help fight the cancer. “Therefore these patients have a better chance of responding to immunotherapy,” says Daniela Thommen, first author of the study.
Increasing the success rate
At present, still only a fraction of patients respond to immunotherapy. “If we could tell from the outset who the therapy will work for, we could increase the success rate. That would reduce side effects and also lower costs,” says Zippelius.
The new findings will enable researchers to develop a practical tool that could ultimately help doctors to decide which patients will benefit from a simple immunotherapy approach and which will require more intensive treatment – for example a combination of chemotherapy and radiation. For that to happen, researchers must first find a way of distinguishing patients based on the amount of PD-1 in their immune cells.
Immunotherapy is becoming increasingly important. “What’s revolutionary about it is that some patients may remain cured after years of treatment – even in the case of tumors that have otherwise proved resistant to therapy,” says Zippelius. In the meanwhile, University Hospital Basel has set up its own tumor board (a group of doctors with different specialties) for immunotherapy.
The study, which was published by the journal Nature Medicine, was led by the Department of Biomedicine at the University of Basel and the University Hospital Basel (USB). Other parties involved were the Department of Medical Oncology and the Department of Thoracic Surgery at USB, the Netherlands Cancer Institute in Amsterdam as well as the Department of Pathology at the Cantonal Hospital Baselland in Liestal and the Roche Innovation Center.
Original source
Daniela S. Thommen, Viktor H. Koelzer, Petra Herzig, Andreas Roller, Marcel Trefny, Sarah Dimeloe, Anna Kiialainen, Jonathan Hanhart, Catherine Schill, Christoph Hess, Spasenija Savic Prince, Mark Wiese, Didier Lardinois, Ping-Chih Ho, Christian Klein, Vaios Karanikas, Kirsten D. Mertz, Ton N. Schumacher, and Alfred Zippelius
A transcriptionally and functionally distinct PD-1+ CD8+ T cell pool with predictive potential in non-small-cell lung cancer treated with PD-1 blockade
Nature Medicine (2018), doi: 10.1038/s41591-018-0057-z
Further information
Prof. Dr. Alfred Zippelius, University of Basel/University Hospital Basel, Department of Biomedicine, tel. +41 61 328 60 16, email: alfred.zippelius@usb.ch