“It may be possible to prevent MS by means of vaccination.”
A large-scale study in the scientific journal Science reveals that the Epstein-Barr virus responsible for causing glandular fever is involved in the development of multiple sclerosis. Professor Jens Kuhle, who participated in the project, summarizes the results in an interview.
13 January 2022
Professor Kuhle, almost everyone is infected with the Epstein-Barr virus (EBV), usually without symptoms. Why does multiple sclerosis (MS) nevertheless occur in a small number?
We know from earlier studies that there are about 200 risk genes for MS. Each of these genes has only a very small effect in itself, but in unfavorable combinations they significantly increase the risk of developing this nerve-damaging autoimmune disease. However, environmental factors always play a role, such as vitamin D deficiency or as in this case potentially a viral infection. It may take certain genetic conditions in combination with the EBV infection for a person to develop MS.
How did the project team come to investigate this virus as a possible cause of MS?
Experts have long suspected that a viral infection could be the trigger. It is known, for example, that children and adolescents who contract glandular fever from an EBV infection have about a twofold increased risk of developing MS later. The research team at Harvard led by Alberto Ascherio, who was in charge of the study now published, had already gathered initial evidence for EBV as a factor in the development of MS in earlier smaller studies. Following analysis of a data set of about 10 million members of the US military, we are now suggesting for the first time that a causal relationship is highly likely. (See box)
How would you describe the mechanism of how exactly this virus triggers MS?
There are several possible explanations. On the one hand, the Epstein-Barr virus may directly attack the nerves and alter them in such a way that the immune system begins to attack the myelin sheath, i.e. the protective layer of the nerve cell processes. This would then lead to the damage and destruction of the myelin sheath that is typical of MS. On the other hand, it could be a case of “molecular mimicry”, in which components of the virus resemble those of the myelin sheath. If the immune system recognizes and fights the virus, the immune cells may then also mistakenly identify the body’s own protective layer as foreign and attack it. But future studies will be required to determine exactly how EBV contributes to the development of MS. These are just two of a number of possible explanations that are currently being investigated.
Multiple sclerosis is two to three times more common in women than in men. How does this fit with the role of the virus as a trigger?
We don’t know as yet. This gender difference is generally still a big mystery. We suspect, for example, that estrogen can actually have a protective effect. So why does MS affect women more often? The answer could lie in the fact that women may be more likely to be deficient in vitamin D, which is also a risk factor for MS. However, it is also conceivable that the Epstein-Barr virus affects the immune system of men and women differently.
Most adults are already infected with EBV. Could and should we protect children from infection to prevent them from getting MS?
As you said, almost all of us are infected with EBV, and the majority of us will not develop MS. Our finding that EBV plays a role in MS is therefore no reason to panic. However, EBV can also have other harmful long-term effects, such as certain cancers. This virus does nothing good for us humans, and a vaccination would be desirable. Such vaccines are currently under development. It might then even be possible to prevent MS through vaccination.
What do you believe the results mean for people with MS?
There is at least a possibility that EBV plays a role not only as a trigger for the condition, but also in triggering disease activity. Little or no data is available on this so far. If this suspicion is confirmed, antiviral therapies, similar to HIV, could be used to get MS under control. Current treatment methods mainly focus on suppressing the immune system in a more or less specific manner. However, as a result those affected can become more susceptible to infection or less able to build up protection against coronavirus, for example, despite vaccination. Antiviral therapy would of course be a highly promising alternative.
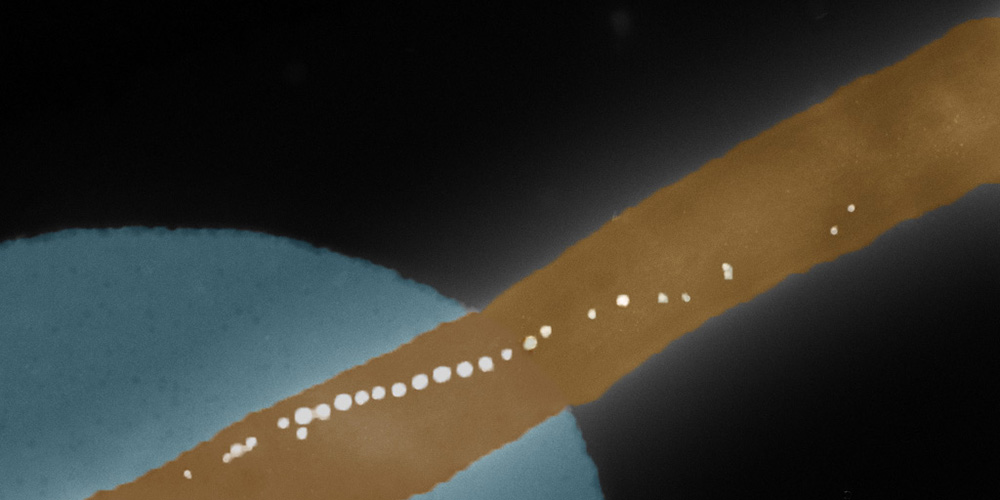
Tracing the role of the Epstein-Barr virus
In order to test for a causal link between the Epstein-Barr virus and multiple sclerosis, the international research team drew on a large US military biobank, which stores blood samples collected over the course of several years from about 10 million military personnel. By analyzing samples collected at the beginning of the subjects' military service and then at two-year intervals, the researchers were able to demonstrate that in almost all cases, the first signs of MS in the blood were preceded by an EBV infection. Of 35 people who were EBV-negative at the time of the first blood sample and later developed MS, 34 had become infected with EBV before the onset of MS. In parallel, but before the initial onset of symptoms of MS, these individuals also showed elevated levels of neurofilament light chain (NfL), a highly sensitive biomarker for nerve damage typical of MS. What is also interesting about the current study results is that no such association with MS was found for another, equally common virus called cytomegalovirus (CMV). This supports the assumption that EBV plays a special role in the development of MS and is in line with earlier data from the Basel research group, which showed increased immune responses to EBV, but not to CMV, in patients with first symptoms of MS.