11.8 million CHF for clinical trials of novel arthritis repair

Swiss government and European Union award 11.8 million CHF for next generation clinical trials of novel arthritis repair. The researchers at the Department of Biomedicine, University of Basel and University Hospital Basel, are actively recruiting for clinical trials.
15 November 2023
The Department of Biomedicine at the University of Basel and the University Hospital Basel, have announced that it delivered the first surgical procedure to treat Osteoarthritis (OA) in humans. The procedure called Nasal Chondrocyte Tissue-Engineered Cartilage, or N-TEC, provides an innovative alternative to cure confined knee cartilage lesions as well as to address degenerative OA cases that have to date required knee joint replacements – prosthetics that routinely need replacing after 15-20 years.
The team at Basel is spearheading the next-generation human clinical trials that will take place at multiple sites across Europe, including Switzerland, Germany, Italy, Croatia, Sweden, Austria and Poland. The Swiss government and EU have awarded the N-TEC program $13.1 million (11.8 million CHF) in funding for these OA clinical trials – and the team is continuing to seek additional funding to expand these trials and deliver this promising regenerative OA treatment to joints other than knees. These clinical trials are open to qualified patients from around the world, including the United States.
According to the U.S. government, there are 2.5 million* joint replacement surgeries in the United States each year and even more patients are looking for alternatives to delay or avoid a prosthesis. Chondrocytes are the cell building blocks for cartilage and the University of Basel team is using them to grow new cartilage. Implantation of this tissue engineered cartilage graft in cartilage defects of the knee could represent an alternative for all patients that need more than simple pain management, but do not want a prosthesis. N-TEC is not appropriate for treating rheumatoid arthritis. The N-TEC current trials will focus only on patellafemeral OA, rather than full knee OA.
The N-TEC procedure was developed by an interdisciplinary research team headed by biomedical engineer Professor Ivan Martin, PhD, director of the Department of Biomedicine, and Dr. Marcus Mumme, MD, senior physician of orthopaedics at the University Children Hospital Basel.
Regenerative Medicine Real in the Clinic Today
Moving beyond trials in the lab and in animals, N-TEC has already taken regenerative medicine in cartilage injury treatment from a lab concept to real clinical success in humans. Leading an international clinical trial with five centres in Europe, the University of Basel team has successfully treated more than 100 patients for focal lesions – 2 to 8 cm2 dimensions – in the knee since 2012, and those patients have already returned to robust sporting activity, including skiing and running half marathons.
Expanding beyond focal lesions six years ago, the University of Basel team treated two patients with advanced knee OA – patients who had been scheduled for knee joint replacement. Those patients, treated with N-TEC and correction of the leg axis, have reported beneficial outcomes (standardized, self-assessed questionnaires) and are still able to perform daily life activities six years postoperative, without the need to resort to artificial joint replacement.
Moving to address OA and cartilage defects in other joints, the University of Basel team is conducting human clinical trials focused on Patella-Femoral OA (PFOA) in the knee and cartilage lesions in the ankle and shoulder joints. They will kick off trials in the elbow joint in 2024.
“I’ve always been a very active, sporty person,” said 56-year-old Marlies Ruckstuhl of Basel, Switzerland. “A fall on ice damaged the cartilage in my left knee and left me with significant knee pain – and a compromised quality of life. Sports were out – and even sitting in my office chair was torture. I was told I needed a knee replacement. In May of 2017, I underwent the N-TEC procedure. After one year of structured physio therapy, I was back to running again, and I went skiing in the winter of 2018. Today, I am back to my old self, pain free and unrestricted – enjoying half marathons and trail running. Life is a pure joy again. A huge thank you to the team at Basel – Bravo!”
Nasal Cartilage – Extracting, Growing, and Attributes
N-TEC is an autologous procedure that relies on cartilage cells from each patient’s own body to grow new cartilage grafts that are surgically implanted to repair damaged cartilage in that patient’s joints. The team extracts a 7x7 mm segment of cartilage from the patient’s nasal septum, isolates and expands the cells, and then grows the cells on a collagen membrane in the lab to create a new engineered nasal cartilage graft of up to 40 cm2. It takes four weeks to grow the cartilage grafts in the lab. The cartilage harvesting from the nasal septum does not damage the patient’s nose.
Importantly, nasal cartilage is comprised of neural crest-derived cells – the type of cells that create higher functioning organs, such as the brain and eyes. These cells are superior to cells from other body parts in the regenerative capacity and in the so-called environmental plasticity – namely, the ability to adapt to different environments and conditions. In particular, nasal chondrocytes, even from older donors, can be reproducibly used to engineer N-TEC cartilage patches that possess structural and mechanical properties typical of articular cartilage tissues.
However, while replacing damaged cartilage in a joint is remarkable, it is not sufficient to fix joint degenerative conditions, such as OA. OA is associated with wear and tear in the joint, as well as with a significant amount of inflammation in damaged joints. That inflammation is a risk factor to break down new cartilage, as it did the original cartilage. In lab and animal experiments N-TEC nasal-engineered cartilage has been proven to possess anti-inflammatory attributes that resist damaging inflammation in repaired joints. N-TEC has also proven its durability in the treatment of OA knee cartilage conducted six years ago.
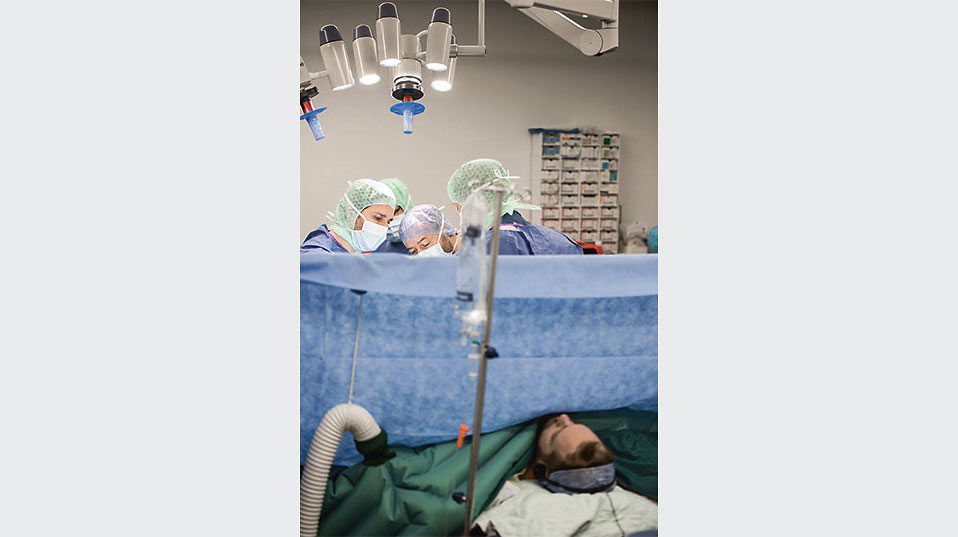
Surgical Procedure
The N-TEC graft is delivered to the joint in open surgery – and the team tailors the new cartilage graft in the operating theater to the shape and size of the cartilage defect. The surgeons suture the graft to the surrounding cartilage tissue. Subsequently, the cartilage integrates with the surrounding cartilage and subchondral bone. The patients are hospitalized for three to five days and the leg is immobilized for the first week post operation. Subsequently, the patients are walking with crutches for an additional six weeks, while the leg is mobilized and the range of motion increased. After one additional week, the patients put their full weight on the leg and continue physical therapy to strengthen the leg. The patient can return to light sports (no impact sports), such as swimming and cycling, after three months, and get back to full robust practices, including sports, after one year.
“N-TEC has demonstrated overwhelming success in human clinical studies to date,” said Ivan Martin, PhD, Professor of Tissue Engineering at the Department of Biomedicine, University of Basel and University Hospital Basel. “Thanks to generous public funding and cooperation with other outstanding teams, we will now extend clinical trials to investigate N-TEC in more challenging conditions so that someday it can become a mainstream bed-side procedure for many patients suffering from joint pain induced by cartilage loss.”
“The amazing N-TEC procedure is funded by grants from the Swiss National Science Foundation and the European Union – and private donors can step up to donate and accelerate N-TEC’s path to the bedside,” said Steve O’Keeffe, founder, Angry@Arthritis, a non-profit focused on attacking and eliminating osteoarthritis, headquartered in Alexandria, Virginia, in the United States. “When the doctor told me I had arthritis it felt like my life as I knew it was over. The team at the University of Basel are providing folks like us with new hope. They actually inspired me to set up Angry@Arthritis – and start my journey toward finding and funding cures for OA.”
*Advanced Research Projects Agency (ARPA-H) Novel Innovations for Tissue Regeneration in Osteoarthritis
Photos and an explanatory video are available for download.