New treatment concepts for recurrent lymphoma
Text: Yvonne Vahlensieck
Cancer recurrence is not always what it seems, at least not in lymphoma, or cancer of the lymphatic system. A study conducted at the Institute of Pathology of the University of Basel has revealed how the genetic profiles of tumors could, in the future, help identify the appropriate therapy for each patient with lymphoma relapse.
What is the probability of a person developing two separate cases of the same type of cancer? Significantly higher than you would think. In some types of cancer, the phenomenon has been known for years. For instance, high exposure to UV radiation during a person’s childhood especially can cause them to develop melanoma more than once in their lifetime.
By contrast, the possibility of two tumors of the lymphatic system (lymphoma) originating independently in the same patient has been rarely taken into account. If a patient develops a second lymphoma, oncologists will often assume that it is directly derived from the first one. The standard treatment for recurrent lymphoma – a combination of aggressive chemotherapy and an autologous stem cell transplantation – is both burdensome for the patient and risky. The chance of surviving a recurrence is only 25 percent.
Understanding recurrence
There is hardly any research on whether recurrent lymphoma necessarily originates from the primary tumor and, particularly, whether aggressive treatment is always the best option. Yet, the need for such research is growing: In the past decades a dramatic increase in lymphoma incidence has been noticed. At approximately 1,700 new cases per year, it is currently the sixth most common type of cancer in Switzerland.
Against this backdrop, Basel University’s and University Hospital’s Institute of Pathology recently investigated the genetic landscape of recurrence of the most common subtype of lymphoma. Professor Alexandar Tzankov and his team analyzed tumor tissue samples from 20 patients with recurrent diffuse large B-cell lymphoma. This type of cancer is considered particularly aggressive. Nowadays, thanks to advances in therapy, 70 percent of patients survive, whereas 30 years ago the survival rate was as low as 20 to 30 percent.
«In the past, the majority of patients died before there was any chance of recurrence», Tzankov explains. In fact, one reason why there is so little research on recurrences of diffuse large B-cell lymphoma is that pathologists could not find enough patients to work with. Which is why Tzankov counts himself lucky that the University Hospital’s archives contained 20 suitable pairs of specimens: tissue samples from patients’ primary and recurrent tumors.
Tracing tumor ancestry
As part of the study, the researchers performed several kinds of genetic analysis to determine the relationship between the respective first and second samples. The team started by identifying genomic regions where genetic material had been lost, duplicated or rearranged. Such irregularities occur in all tumor cells, giving each tumor a genetic profile that is as unique as a fingerprint. In a second step, they sequenced specific sections of DNA that are often mutated in lymphoma and documented subtler alterations.
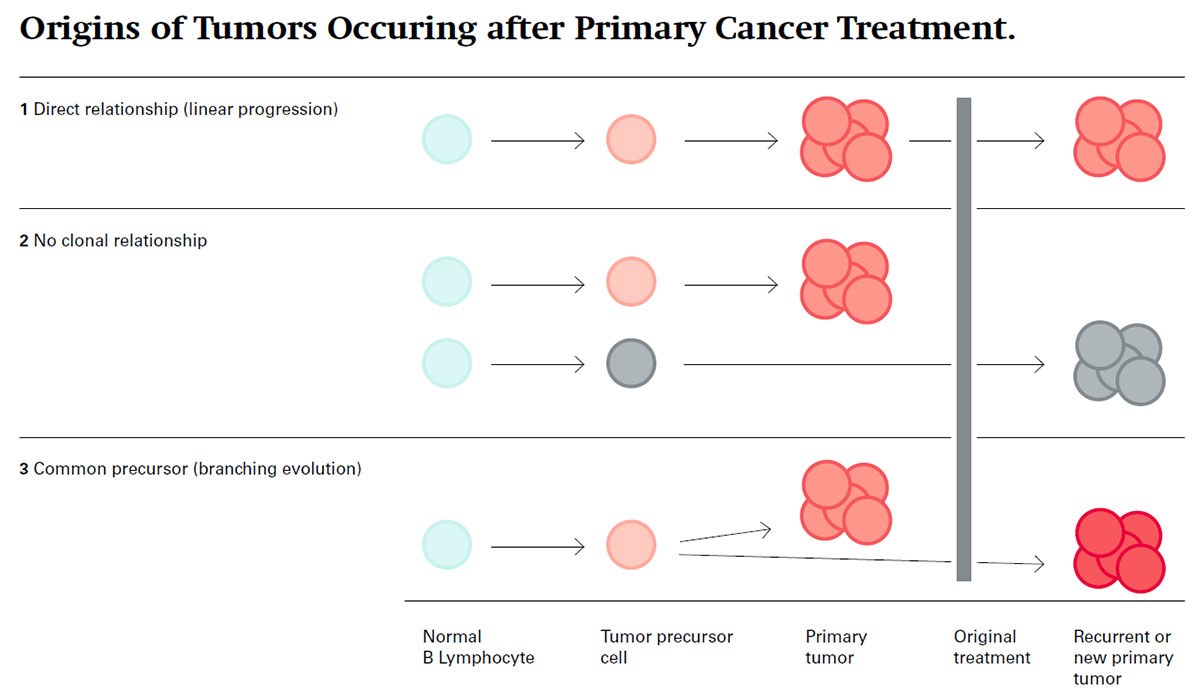
Analysis of the data yielded insight into the tumor ancestry. It was found that a tumor appearing after primary cancer treatment can have at least three different origins: the two tumors can be directly related, indirectly related or unrelated. Eleven of the 20 sample pairs were directly related, meaning that the second tumor clearly originated from the first one as a kind of «linear progression», as had been expected. When that is the case, the conventional aggressive treatment approach seems sensible, as the recurrent tumor is likely to consist of cells that have become resistant to the original chemotherapy.
However, three sample pairs showed virtually no shared genetic alterations. In other words, the corresponding patients had not suffered a true recurrence, but rather had developed a new case of lymphoma («clonally unrelated second tumor»). How this is possible is unclear, since little is known about what triggers the disease. Potential risk factors include certain herbicides, genetic predisposition, immunodeficiency and old age – most sufferers are between 60 and 80 years old. The remaining six sample pairs were found to be only indirectly related. While the samples shared some characteristics, there were also significant differences. The most likely explanation is that the primary and secondary tumors originated in the same cell but diverged at a later stage as a kind of «branching tumor evolution».
New treatment concepts
«Between a fifth and a third of sample pairs show no clonal relationship», is how Tzankov summarizes the findings. «And in such cases, I can expect to reconsider treatment options.» This could mean that, in the future, some lymphoma patients would not have to undergo treatment that is both grueling and risky. However, Tzankov stresses that findings from such a small case series are not a sufficient basis for changing proven treatment approaches: «All new therapies need to be tested in properly designed large-scale studies. What we do hope is that our findings have sparked the interest of other researchers and that the question we’ve raised will feed into the design of upcoming prospective studies.»
Nonetheless, pathologists at Basel now routinely determine the precise genetic profiles of recurrent lymphomas for diagnostic purposes, and this has already benefited a number of individual patients. Tzankov cites the case of a colleague’s terminal patient for whose recurrent lymphoma all conventional treatment options had been exhausted over the course of two years: «Since the potential recurrence was demonstrably unrelated to the first tumor, she was considered eligible for a completely different type of therapy. The patient seized the opportunity and survived. Three years on, she’s still doing well.»
More articles in the current issue of UNI NOVA.