Testing cancer treatments on mini-tumors.
Text: Catherine Weyer
Raphaëlle Servant creates tumors in miniature. The doctoral researcher wants to use these organoids to make personalized cancer therapy possible.
For Heiner Schläpfer, it started with blood in his urine. His doctor diagnosed prostate cancer. This was followed by a prostatectomy – the removal of the whole prostate – chemotherapy and chemical castration. Generally, this a good way of treating prostate cancer. Chemical castration stops the cancer cells getting any more testosterone, so they are unable to continue growing and die off.
But then Heiner Schläpfer gets some bad news. The cancer is back; the treatment hasn’t worked. Worse still, the cancer is now more aggressive than before. A new kind of therapy is needed.
Every day there are cases like that of the – fictional – Mr Schläpfer in Switzerland. Raphaëlle Servant wants to use her research into prostate cancer cells to help those affected. Servant is a doctoral researcher at the Department of Biomedicine in the group led by Clémentine Le Magnen, whose aim is to understand each individual’s cancer better.
After Heiner Schläpfer’s cancer returns, his urologists take a biopsy of the tumor and send it to pathology. There, the pathologists examine the tissue sample and pass on a section containing tumor cells to Raphaëlle Servant and her colleagues. She extracts parts of it for analysis and for organoids. These are essentially mini-tumors grown in the lab that are designed to be as similar as possible to the original.
An exact copy of the tumor
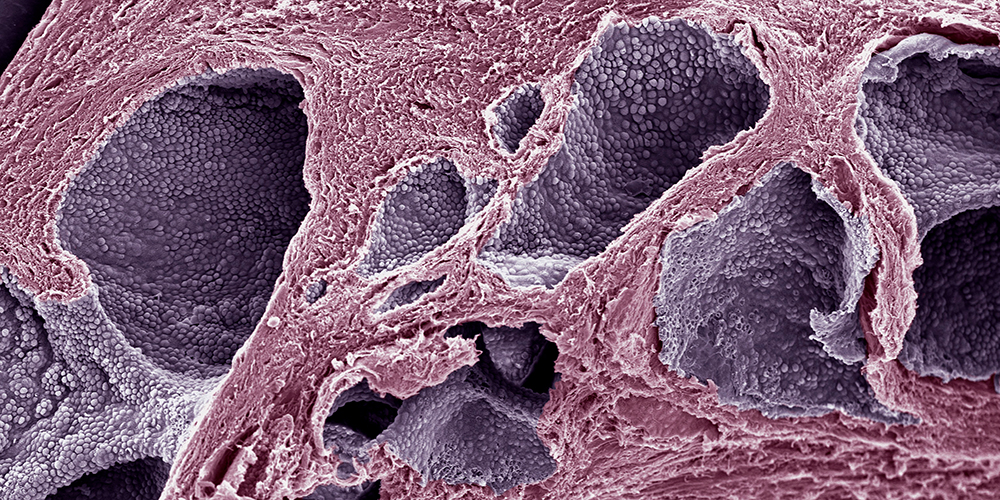
To harvest these organoids, a section of the tissue biopsy is dissected into individual cells. Then Servant places them in a petri dish, in a gel-like matrix that allows the cancer cells to grow in 3D. In a nutrient solution containing different growth factors, small spheres gradually form. Ideally, these will be exact copies of the original tumor.
In the long term, these organoids should help us to test different treatments for the specific cancer in advance in the lab to identify the one that produces the best possible outcome for the patient. This translational research project is only made possible by the collaboration between urologists, pathologists and researchers. Had this option been available to Heiner Schläpfer, it would have given him a personalized solution, tailored to his unique cancer.
As yet, however, the researchers have not reached that stage. As Servant notes, prostate cells are very heterogeneous, so it’s difficult to get hold of the right ones — those that have mutated into cancer cells. “It takes several weeks for the organoids to grow large enough for us to be able to examine them. And then we often find that we haven’t got hold of cancer cells, but rather benign cells.” If all goes well, it takes around a month for the organoids to reach a suitable size, which is about 50 micrometers in diameter. “Currently, this is only the case with one in five of our samples,” Servant estimates.
Research into prostate, kidney and bladder cancer
A significant part of her work is therefore about identifying good growing conditions for the prostate cells so that they thrive in the petri dish, since this is where the difficulties start. The great upside to prostate cancer is that it grows slowly, but this is also its downside.
It means that the researchers have considerable time, relatively speaking, after the prostate biopsy to analyze the tumor before the patient’s cancer progresses too far. On the other hand, it also takes a long time for the organoids to become large enough to be tested. Along with prostate cancer, Clémentine Le Magnen’s research group is investigating kidney and bladder cancer, both of which are also types of cancer that grow relatively slowly.
If Servant is successful and the cancer organoids grow, she can test out therapies on them. The tests involve administering different cancer drugs and working out the optimal dosage of the optimal agent.
Servant sums it up like this: “After putting in a lot of time and effort to work out how the cells grow best, we want to examine how best to kill them off.” She goes on to explain, “There are 1,500 chemical compounds that are suitable for use as cancer drugs.” And it is the characteristics of each specific tumor that determine which combination of substances will be most effective.
The researchers can now use automation to test the drugs. A device resembling a small printer can inject the different agents into the individual petri dishes in precisely defined quantities. If the tumors die off, the researchers know that the drug is effective. And by varying the dosages, they can gauge how much of it is sufficient to eradicate the cancer cells without causing unnecessary damage to the healthy cells.
Looking for the cancer signature
Heiner Schläpfer was affected by a well-known problem in cancer treatment: the return of the cancer in a form resistant to treatment. The researchers are still trying to figure out why that happens. Within the research group, the person charged with tackling this problem is the postdoc Romuald Parmentier.
Parmentier analyzes the mRNA of each individual cell of the organoids and tumors to determine their precise composition. The researchers hope to be able to draw conclusions from this. If resistant cancer cells exhibit a particular signature, that information can be used to work out whether or not chemical castration will be sufficient to deal with a tumor. Treatment can then be adjusted accordingly.
It will probably be some time before the research group is able to make treatment recommendations to attending physicians. Raphaëlle Servant, however, will be finishing her doctorate shortly. She is optimistic that she is on the right path. “We’re learning more and more about the organoids and how they grow best. Once we have optimized that part of it, we’ll be much closer to the solution.”
Raphaëlle Servant is a doctoral researcher at Basel University’s Department of Biomedicine. She is studying the mechanisms that drive prostate cancer. Her research group led by Clémentine Le Magnen is also part of the Institute of Pathology and the Department of Urology at Basel University Hospital.
More articles in this issue of UNI NOVA (May 2023).