Extinguishing fires in the brain.
Text: Ori Schipper
People researching puzzling diseases such as multiple sclerosis are constantly making unexpected discoveries, such as immune cells from the intestine that migrate to the brain – where they relieve inflammation.
Multiple sclerosis (MS) is known as the “disease of a thousand faces”, because its symptoms differ considerably not only from one person to another but also within the same person depending on the severity of the disease and from one day to another.
“We see patients who are still running marathons, even at an advanced age, as well as others who are in a wheelchair just a few years after being diagnosed with MS,” says Anne-Katrin Pröbstel, research group leader at the Departments of Biomedicine and Clinical Research of the University of Basel and senior consultant at the Department of Neurology of the University Hospital Basel.
Misdirected immune cells
Perhaps even more mysterious than the many faces of this disease are its origins. Although scientists agree that MS is an autoimmune disease in which misdirected immune cells from the patient’s own body attack the central nervous system, it remains unclear how and why this takes place – despite decades of intensive research. For a long time, the focus of research was on T cells, which make up some 80 percent of all immune cells. Over 30 years have passed since researchers first linked T cells to inflammatory diseases in the brain based on experiments on mice.
The significance of the other large group of immune cells, the B cells, didn’t become apparent until much later. This discovery came in the form of a notable clinical trial in 2007, whose results showed that a drug that targeted B cells led to an almost total reduction in inflammatory lesions. “The findings were sensational,” recalls Pröbstel. Previous drug trials had all reported a much smaller reduction in inflammation. Analyses of the patients’ blood and cerebrospinal fluid found that traces of B-cell activity had not completely vanished, however, and that although the active substance eliminated many B cells, it didn’t get rid of them all.
On the back of these findings, researchers developed another drug with a broader spectrum of action – and that targeted all B cells without exception – but the ensuing trial of this new active substance ultimately resulted in failure. “Instead of reducing the number of inflammatory sites in the brain, the treatment led to a greater number of flare-ups. No one understood why at the time,” says Pröbstel. It would be another five years before she and her colleagues stumbled across a possible explanation for the disappointing results.
Comparison of stool samples
Before taking up her current position in Basel in 2019, the physician and researcher worked in San Francisco, where she focused on the interaction between B cells and microbes in the human intestine.
Previous studies had already demonstrated that these tiny creatures in the digestive tract influence the development of MS. By analyzing the intestinal flora of MS patients and healthy individuals, researchers had detected differences in the composition of the microbial community. Meanwhile, other experiments had shown that these differences were relevant to the disease. Specifically, when researchers transplanted stool from MS patients into the intestines of mice, it led to inflammation in the rodents’ central nervous systems.
“The B cells in the intestines secrete antibodies, thereby ensuring a balanced intestinal flora,” says Pröbstel. Theoretically, these cells should have a lot of work to do, particularly during an acute episode of MS, but when Pröbstel’s team compared stool samples from patients experiencing a flare-up with those from individuals whose disease was dormant, the results came as a surprise. Stool collected in an acute phase actually contained fewer – not more – antibodies than that collected when the disease was not apparent. “We asked ourselves, where have all the B cells gone then?” says Pröbstel.
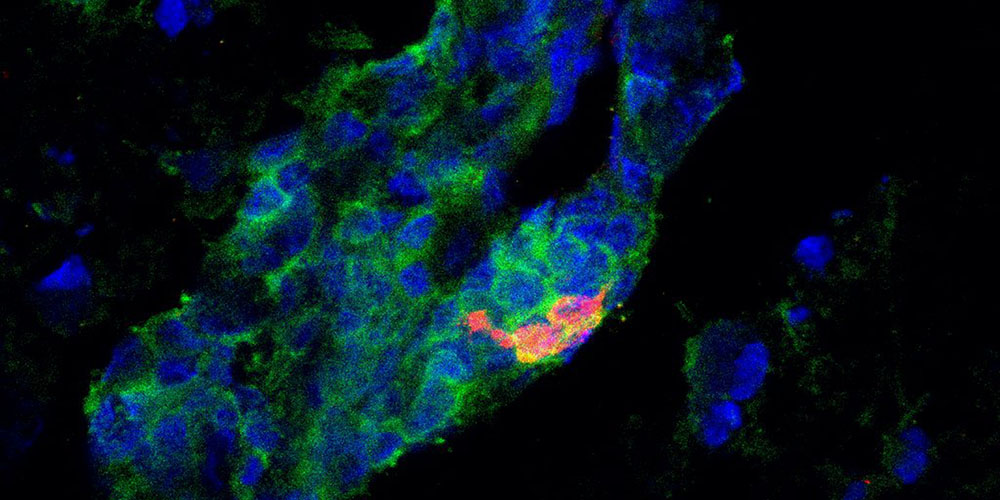
Further experiments found that, in acute phases of the disease, the B cells in the intestine migrate from the digestive tract into the central nervous system, where they reduce inflammation. “We didn’t expect that. It seems there are not only bad B cells that cause flare-ups of the disease, but also good ones that keep inflammation in check,” says Pröbstel. Accordingly, one possible explanation for why the active substance with the broader spectrum of action performed so badly was probably that it eliminated not only the bad, but above all also the good B cells.
Immune cells swarming out of the intestine
Pröbstel thinks that B cells from the intestine might play a similar protective role in other autoimmune diseases – such as type 1 diabetes, systemic lupus and rheumatoid arthritis. Her team also recently stumbled across intestinal B cells in the cerebrospinal fluid of patients suffering from serious neurological consequences following a Covid-19 infection.
Pröbstel describes the B cells from the intestine as “a sort of fire department”. When everything in the body is in order, they remain in the intestinal mucosa and work to keep the huge variety of microbes in a state of healthy equilibrium. When an inflammatory response flares up in a specific part of the body, however, the B cells swarm out of the intestine in order to extinguish the fire.
Through their work, Pröbstel’s research group are contributing to a deeper and better understanding of the development of multiple sclerosis. Moreover, the physician and researcher hopes that these findings could lead to the development of novel treatment approaches. For example, she can imagine future treatments in which patients are given selected intestinal bacteria that cause good B cells to multiply in the intestine, essentially bolstering the B cell fire department so that it can bring outbreaks of fire under control as quickly as possible.
More articles in the current issue of UNI NOVA.