When the virus returns.
Text: Ori Schipper
Immunological memory is based on complex interactions between different types of cells, and the process involves thousands of genes. Two perspectives on a fascinating phenomenon with which scientists are still struggling to come to grips.
It’s never happened so fast before. Thanks to the tireless work of countless research groups, it was possible to develop an effective vaccine against the SARS-CoV-2 coronavirus within the span of just a single year. Widespread vaccine campaigns have already begun to roll out, but the pressing question now is: How long will the vaccine protect us? Will it be effective against the mutant variants of the coronavirus now emerging in multiple countries around the world?
“The aim of every vaccine is to produce an immunological memory that lasts as long as possible,” says Carolyn King, Research Group Leader at Basel University’s Department of Biomedicine. The idea is to expose an individual to a pathogen that has been weakened or split up into benign subunits with the goal of eliciting a response from the immune system. How effective the immune system is at fighting off this particular pathogen or a related mutant strain depends on the interaction between the different immune cells that are activated by the defensive response – and that remain active after the infection subsides.
Today, there are a wide range of established vaccines. But many questions regarding the exact role of different cell types in building immunological memory remain unanswered. This is a point of serious contention for experts in the field. The fact of the matter is that these details are not only important to researchers; they are critical to the development and production of vaccines, too.
What we do know is that the typical immune response is divided into two phases: The “innate immune response” is rapid, attacking many foreign pathogens just minutes after they enter the organism. However, this type of response is non-specific and fails to form any long-term immunological memory. Memory is formed in the second phase, during the “adaptive immune response,” in which the immune system launches a targeted assault against a specific pathogen.
Quicker and more efficient response
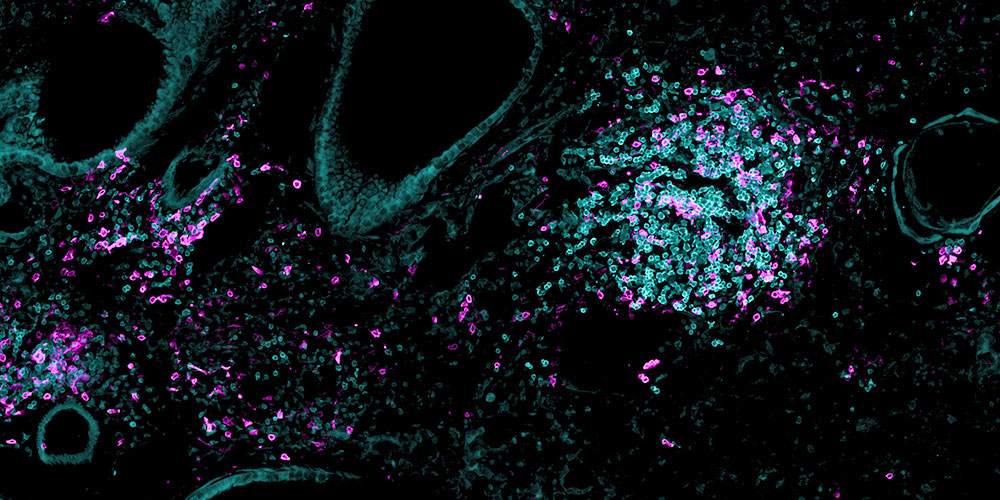
Central to this adaptive immune response are the interactions between the different types of immune cells, which can be roughly split into three categories: B cells, helper T cells and killer T cells. B cells are primarily associated with the production of antibodies, which bind to specific pathogens, thereby placing a kind of chemical target on the invader. Helper T cells release signal molecules to help support other immune cells, and killer T cells are deployed to destroy infected cells.
Humans are born with T cells featuring a multitude of different receptors, or uniquely shaped sensors located on the outer surface of the cell. So, when an infection occurs – or a vaccine is injected – the immune system activates only those specific T cells with receptors capable of binding to the corresponding parts of the pathogen. These T cells then multiply in order to mount a battle against the foreign body. After their work is finished, most activated defensive cells die off, while a small number remain alive in the host. These “memory cells” ensure that the organism’s immune system is able to respond quicker and more efficiently the next time that same pathogen is detected in the body. “Research on T cell memory has long been focused on killer T cells,” says King.
The lung’s memory
King and her team are primarily interested in helper T cells. Their main function is support the production of antibodies by B cells. It has long been known that T cell help to B cells takes place in either the spleen or the lymph nodes. However, after conducting a number studies on mice and influenza viruses, King’s team was recently able to conclude that T cell help to B cells also occurs in lung tissue.
Surprisingly, helper T cells remain in the mucous membranes of the lungs long after the infection has been eliminated. There they interact with B cells, allowing the body to prosecute a local defensive re-sponse should reinfection occur. King’s experiments also demonstrated the importance of lung resident helper T cells in orchestrating an effective immune response against closely related variants of influenza viruses.
Clearly, the body not only maintains a fleet of memory cells that circulate in the blood; it also stations a squad on the frontline – in the tissue where the same or a similar pathogen may reinfect the body – to serve as a memory of the initial infection. “The longevity of these helper T cells in the lungs and their ability to respond quickly to infections by mutated pathogens make them a promising candidate in the search for vaccines that off er lasting protection,” remarks King.
Like clockwork
The immune system’s aptitude for remembering previously-encountered pathogens is also the subject of study by one of King’s colleagues, Mike Recher, who heads up another research group at the Department of Biomedicine and supervises the Clinic for Immunodeficiency at University Hospital Basel. His clinic serves patients suffering from frequent recurrent infections.
Many thousands of genes are involved in the structure and function of our immune system. So, according to Recher: “It’s no wonder that immune deficiencies often stem from genetic changes.” Recher illustrates the effect of a mutation by drawing an analogy: “All these genes are like sprockets in the complex gear system that make up a mechanical clock. If just one of those sprockets refuses to bite, the whole clock stops ticking.”
Even though defects can impact different genes (or sprockets), the effect is the same for over half of Recher’s patients: Their immune systems are unable to produce a sufficient number of antibodies. This ’immunoglobulin deficiency’ often causes recurrent respiratory infections. However, according to Recher, infections can be prevented using immunoglobulin replacement therapy, a treatment method with a long history and track record of success.
It only takes a few drops of blood to determine whether a patient is low on antibodies. The test is simple and affordable, adds Recher. “But it takes an average of ten years before doctors are able to isolate the cause of a patient’s health problems.” By then, untreated immune deficiencies can result in irreversible organ damage. That is why Recher considers it crucial to focus not only on immunological memory, but on the memories of medical practitioners, too. Doctors must consider the possibility of immunodeficiency early on, so that patients with suspected cases can be tested sooner rather than later.
More articles in the current issue of UNI NOVA.