When sleeper cells cause problems
Karin Bundschuh
Infectious diseases are becoming increasingly hard to treat. Slow-growing bacteria in particular are making therapy difficult.
There is a fair amount of injustice among infections. Some pathogens enjoy perfect conditions. They have all the nourishment they need and can reproduce in their millions. Meanwhile, entirely identical bacteria in the immediate vicinity end up starving and can multiply only at a sluggish rate.
These unequal conditions in one and the same organ are significant not just for the bacteria, but also for their host. While one course of antibiotics is usually enough to put a stop to rapidly reproducing germs, their slow-growing compatriots can endure high concentrations of antibiotics over days, weeks or even months without any sort of permanent effect. Dirk Bumann and his team have shown how this leisurely development allows them to elude attacks by penicillin and other medication without being resistant. According to the infection biologist, these “moderate, scarcely even noticeable pathogens” are primarily responsible for the recurrence of infections following antibiotic treatment.
Bacteria grow at different rates
However, Bumann, who has been researching in the Biozentrum since 2007, does not yet know why such unequal conditions occur in infected tissue. To date, little research has been conducted into where bacteria settle within an organ and how they spread within it. “It was thought that it made no difference,” explains the scientist. “Classical anatomy just wasn’t really on our radar for us microbiologists.”
Originally from Berlin, he is sure that this will change. The entire field of research will evolve. In a recent review for the scientific journal Cell Host & Microbe, the professor explains why a new perspective on the relationship between host and pathogen is so exciting and rewarding. If researchers obtain more precise information about what happens to pathogens in different parts of an organ, they may be able to target antibiotic therapies more specifically and provide tailored support to the immune system in its fight again salmonella, staphylococcus and mycobacteria. But before treatment can be improved in this way, many open questions must be clarified.
Why exactly are there such major differences in environment in such a confined space? Tuberculosis is a good example of this phenomenon. “Our immune system manages to kill off many pathogens in the lungs. Directly adjacent, however, the tissue contains active loci that give bacteria access to the airways and can infect many other people,” the researcher reflects. So although the host can defeat a large number of pathogens, ultimately this is not enough, because in some instances the bacteria win. But why do the bacteria ultimately prove superior? Bumann hypothesizes that the immune system often lags a little behind in the fight against rapidly spreading bacteria.
It is also unclear which conditions contain the most pathogens when they infect the tissue. In their examinations of salmonella, the scientists in Basel established that only about 10% of bacteria happen on good conditions and can multiply in an optimal manner. The rest have to contend with a rather inhospitable environment. These pathogens are probably lacking in nutrition while being attacked by the immune system, which attempts to annihilate the invaders with low pH levels, little oxygen, aggressive radicals and defensive immune cells. However, the environment is yet to be analyzed in detail. Clarification is also required as to how infections spread in the tissue. “These questions are fascinating because they are fundamental to achieving better understanding and new treatment options. It will certainly take us many years to answer them all,” surmises the infection biologist, not at all alarmed by the prospect.
Measuring reproduction in the tissue
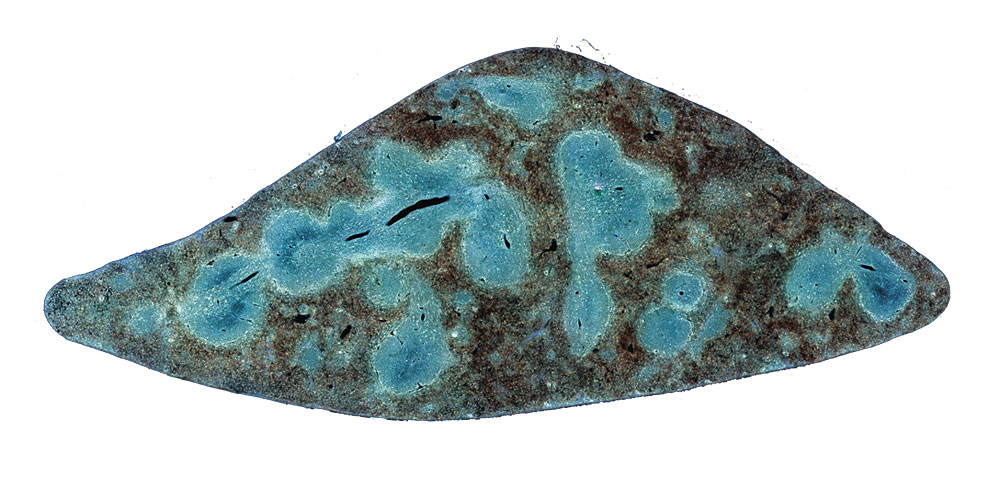
Previously used only in brain research, three-dimensional microscopic processes are providing the researchers in Basel with completely new ways to find answers to their questions. Cutting equipment and a microscope are combined in a device that can analyze and strip an organ slice by slice without deformations. “It’s like looking at sliced bread from above with an unbelievably high resolution,” explains Bumann. Structures separated by just two thousandths of a millimeter can be distinguished using these high-tech devices.
The contrast is boosted with the aid of fluorescent colorant, which illuminates the bacteria in the tissue. This process now works not just with light microscopes, but also with electron microscopes. Although images are provided only in black and white, the resolution is actually in the nanometer range. This allows the membrane surrounding the bacteria to be viewed. It takes three weeks for an organ to be captured and photographed step-by-step, culminating in a terabyte of data. Analyzing this data is one of the greatest challenges for Bumann and his team.