"Many zoonoses are being forgotten in the wake of corona."
Interview: Irène Dietschi
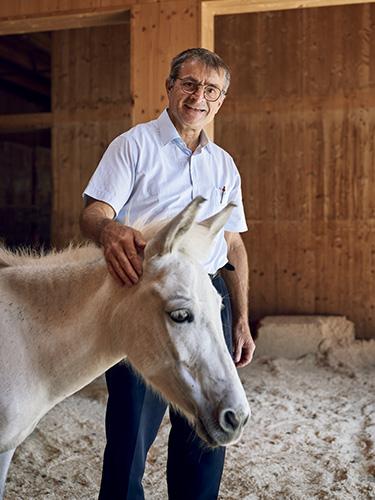
Since the end of the 20th century, a growing number of pathogens are spreading from animals to humans. Jakob Zinsstag studies these zoonotic diseases, or zoonoses, and explores how a new understanding of medicine can help fight them.
UNI NOVA: Jakob Zinsstag, let's start by talking about monkeypox, the infectious disease that is slowly but steadily spreading across the world. There has been a lot of discussion about the name. Why is that?
JAKOB ZINSSTAG: The name is based on a misunderstanding. This virus was first identified in monkeys in 1958, but it was later found to have originated in numerous species of rodents and other wild animals in Africa. Monkeys can become infected, but they are not reservoir hosts for this virus, meaning that they do not spread it to humans.
UNI NOVA: To what extent can we say that this new viral infection is typical of the times we’re living in?
ZINSSTAG: I'm not at all surprised that this virus has emerged. Back in 2005 with the bird flu, we were saying that we have to improve biosecurity between humans and animals, whether that's at wet markets or other spaces in which domesticated animals come into contact with wildlife. By and large, that warning has been ignored. Based on our two and a half years of experience with SARS-CoV-2, which most likely originated in bats, we know full well that pathogens from animals can jump to humans and that this mechanism can bring about a global pandemic.
UNI NOVA: Do we know how long animal pathogens have been spreading to humans?
ZINSSTAG: Zoonoses have been a part of human life throughout our evolution – from our time as hunter-gatherers through to the advent of agriculture. One of the best-known zoonoses is rabies, and even the Ancient Egyptians knew that dogs were involved in that disease. Other zoonoses, such as tuberculosis in cattle or brucellosis, were first discovered in the 19th century, in the time of Robert Koch and Louis Pasteur.
UNI NOVA: Bats have been implicated in countless epidemics such as the human mumps virus and, most likely, SARS-CoV-2, as well. The animals are hosts, but they themselves don't get sick. Why is that?
ZINSSTAG: Bats are the only mammals that can fly. It has been posited that in order to gain this ability they had to eliminate a lot of extra ballast, so they have only a rudimentary inflammatory system. That means that when they get infected, they do not show clinical signs of disease. It's why, in theory, bats can host a large number of viruses without suffering as a result.
UNI NOVA: Which zoonotic diseases have the highest case rates, aside from monkeypox and Covid-19?
ZINSSTAG: There are some very well-known zoonoses, such as Lyme disease, Ebola and rabies, but they aren't the most common diseases. There are far more cases, for instance, of the bacterial infections brucellosis and leptospirosis. These diseases occur the world over but tend to be ignored in "poorer" countries, likely because the course of the disease is slow and relatively inconspicuous. Sometimes they don't even find their way into the list of neglected diseases. But that doesn't mean they are harmless: Brucellosis is a generalized chronic febrile illness that affects almost every organ in the body and causes major losses of livestock in the Global South, principally sheep, goats and cattle. It causes the animals to miscarry. Humans pick up the bacteria through their milk and can also develop diseases, such as Malta fever, as a result. It would be easy to combat brucellosis with a vaccine for livestock and humans. Leptospirosis also causes major problems for livestock and the people who work with them. Even rabies is still a problem. There are hundreds of such diseases that are being forgotten in the wake of the coronavirus pandemic.
UNI NOVA: Rabies, monkeypox and Covid-19 are viral infections. Are viruses the most common pathogens for zoonotic diseases?
ZINSSTAG: Viruses play a major role – probably the most important role when it comes to zoonoses. But there are also many, many bacteria that are zoonotic, for example the pathogens that cause Lyme disease or plague. Even worms can transmit diseases. For example, there is schistosomiasis, which is very widespread in Africa, or dog tapeworm. Even single-celled protists, like the Malaria pathogen or amoebas, can cause zoonoses. The number of zoonoses has risen dramatically since the latter part of the 20th century.
UNI NOVA: Why is that?
ZINSSTAG: Significant factors include the loss of biodiversity, massive deforestation and agricultural use of formerly wild ecosystems. When you have higher species diversity, it is difficult for pathogens to jump between different animals because there are more robust or even resistant species. That means only a portion of the animals are susceptible to the pathogen and able to transmit it. This "thinning effect" disappears as species diversity declines. And it is further weakened by increased contact between humans and wild animals as well as between wild and domesticated animals. Add to that the fact that we humans travel far more. Global air travel has more than quadrupled in the last 15 years alone. Trade in wildlife and wild meat plays a key role, too.
UNI NOVA: How do differences between countries affect the development and spread of zoonotic diseases?
ZINSSTAG: They play a major role. That is the focus of infection ecology: studying the distribution and circulation of diseases – not just in humans, but in the entire social and ecological system. It can vary based on the geographical context. For example, in the case of brucellosis, the disease affects different animal populations in Mongolia and Kyrgyzstan than it does in Mexico or Morocco – and then it spills over from the animals to the human population. The modes of transmission are different, too, depending on cultural practices. In Mexico, for instance, the pathogen is transmitted via milk and dairy products, while in Mongolia it tends to be spread directly from animals to humans.
Here's another example: In Mongolia, marmots carry the bacterium Yersinia pestis, which causes plague, and humans can become infected by hunting these animals. Plague is a problem in Madagascar, too. There, rats and other rodents are involved because the pathogen is spread to humans by fleas. In Switzerland, on the other hand, neither marmots nor rats carry this bacterium.
UNI NOVA: Some zoonoses seem to disappear, like the dreaded Zika virus: A few years ago, pregnant women in Central and South America who had been infected with Zika were giving birth to children with severe brain damage. Other pathogens, like SARS-CoV-2 simply remain in circulation and continue to mutate. What accounts for these differences?
ZINSSTAG: Many diseases are considered "emergent" – which means they develop suddenly due to a complex interplay of ecological factors. These interactions are in constant flux, meaning that pathogens can arise very suddenly and disappear again just as quickly. That seems to have been the case with Zika. Even the outbreaks of Ebola in West Africa – following numerous interventions to quell the epidemic – subsided again on their own, and nobody knows where the virus has disappeared to.
UNI NOVA: Why hasn't Ebola spread to Europe?
ZINSSTAG: The Ebola virus is highly deadly. Anybody who gets infected becomes ill very quickly and is unable to travel. The person has to be treated locally, so the virus remains contained within a small area. A personal anecdote to that point: In 1994, when I was in Ivory Coast managing the Centre Suisse, I experienced a dramatic exception to that rule. One of our students had become infected with Ebola and was in critical condition. Without knowing it was Ebola, we had him emergency airlifted to Switzerland where he received treatment under strict biosecurity protocols and survived. In retrospect, our response was risky, but of course we were relieved that it turned out alright in the end.
UNI NOVA: You are a pioneer of One Health, an approach that could help prevent the emergence and spread of zoonotic diseases. Could you explain what that means?
ZINSSTAG: One Health advocates combining different medical surveillance systems used for wildlife, the environment, livestock and humans. There are successful models for this practice in Europe: In Italy's Emilia-Romagna region, an integrated approach is being used to monitor West Nile virus in mosquitos, wild birds, horses and humans all at the same time. If the virus appears in one of these groups, the other sectors are informed and asked to monitor their populations more closely. This approach has already prevented contaminated blood from being spread among humans via blood transfusion.
UNI NOVA: It is probably not quite so easy to monitor human interactions with wildlife.
ZINSSTAG: That's true. We first have to identify where we can find the information we need and who to contact to get it. In Ethiopia, we’re working with hunters and gamekeepers as part of the Jigjiga University One Health Initiative funded by the Swiss Agency for Development and Cooperation (DEZA). The Swiss Tropical and Public Health Institute (Swiss TPH) has local offices in three districts. These offices have both veterinary specialists and medical personnel on staff and maintain contact with village officials responsible for community and animal health. And if these officials spot a miscarriage in one of their animals or treat a sick child or a sick woman, then they get together to discuss possible zoonotic origins. They take blood samples and arrange to have the patient transferred to a hospital, if necessary. This is how we've been able to establish One Health systems in Africa with relatively little difficulty. It works in Guatemala, too.
UNI NOVA: That's assuming you're able to adapt to local conditions, right?
ZINSSTAG: Correct. If we were to plan our projects while ignoring the people who live there, our initiatives would fail. These types of systems are only accepted at a local level when we include the local population and integrate their non-academic knowledge in our work. We call it a transdisciplinary process. We are also trying to convince local people to work across borders between countries. We illustrated why that would pay off using an approach from game theory: Just recently, we used a model to determine that it would be possible to eliminate rabies in Africa within 30 years by vaccinating dogs, provided that the countries worked together to coordinate their vaccination campaigns. The countries in question would also stand to save a lot of money.
UNI NOVA: Are you fighting a losing battle? What I mean by that is: Will the pathogens always be faster, or are you optimistic that your approach will work?
ZINSSTAG: I’m certainly optimistic. Take coronavirus, for instance: Never before have we been able to vaccinate people against a pathogen so quickly. There may be plenty to criticize about the restrictions that were employed, but the collaborative effort – and cooperation on a global level – was ultimately a good thing, and it was coordinated over large areas. If we are prepared to engage in more effective collaboration between sectors – human medicine, veterinary medicine, environment and agriculture – and if we manage to draft an international convention on pandemics like the one currently under negotiation in Geneva, then I’ll be even more optimistic about the future. And, of course, molecular biology has enormous potential to combat pathogens and prevent potential disease, both on a diagnostic and a therapeutic level. We have a lot of room for improvement in the fields of animal welfare and biosecurity. But the world is prepared to respond to new zoonotic diseases – that's a proven fact.
More articles in the current issue of UNI NOVA.