A fatal mix-up: how certain gut bacteria drive multiple sclerosis
If gut bacteria are too similar to the protective layer of nerves, they can misdirect the immune system and cause it to attack its own nervous system. This mechanism can accelerate the progression of multiple sclerosis, as researchers at the University of Basel have shown in trials with mice. However, their results also open up opportunities for treatments that make use of the microbiome.
15 December 2025 | Angelika Jacobs
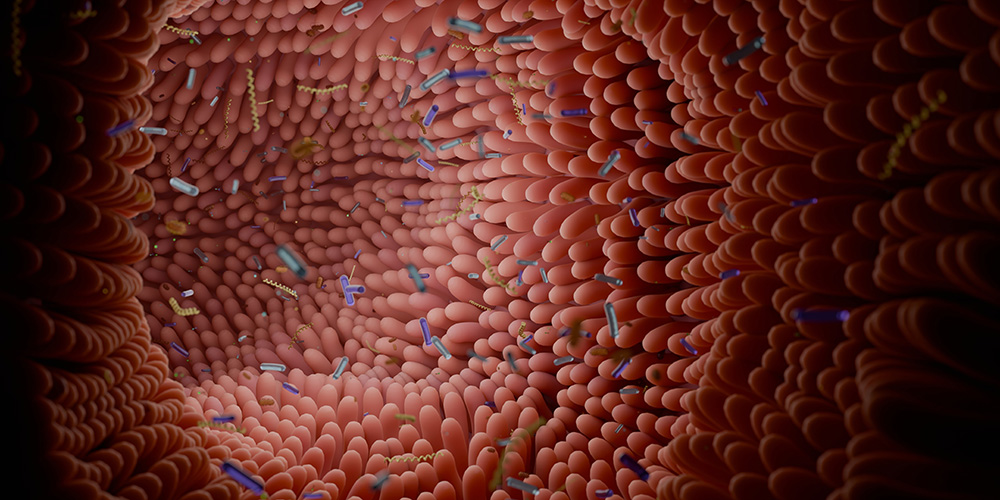
When the immune system confuses friend and foe, autoimmune diseases develop. In the case of multiple sclerosis (MS), it mistakenly attacks the body’s protective layer of nerve fibers, known as the myelin sheath. Those affected can experience exhaustion and numbness in their limbs, develop walking problems and may even become paralyzed.
Researchers have spent decades investigating the question of how this fatal error in our defenses occurs. More recent hypotheses also focus on the intestinal flora. This is because people with MS have a different composition of microorganisms in their intestines than healthy people.
“We know that the intestinal flora influences the immune system, but the mechanisms related to MS are not fully understood,” says Professor Anne-Katrin Pröbstel from the Universities of Basel and Bonn. With her research group at the University of Basel and at the University Hospital Bonn, the neurologist investigates the role of the microbiome in neuroinflammatory diseases.
Dangerous look-alikes
One hypothesis suggests that pro-inflammatory gut bacteria, which have similar surface structures to the myelin sheath of the nerves, upset the immune system. The immune cells then attack both the harmful bacteria and the body’s own myelin sheath. Experts refer to this likeness between bacteria and myelin sheath as “molecular mimicry”.
In a study published in the journal Gut Microbes, Pröbstel’s research team, with lead authors Dr. Lena Siewert and Dr. Kristina Berve, has provided new evidence for this hypothesis. Using molecular biological methods, they modified pro-inflammatory Salmonella bacteria so that they had a surface structure similar to that of the myelin sheath. They used bacteria of the same species without a self-structure as controls.
In genetically modified mice, which can serve as a disease model for MS, the myelin-like Salmonella bacteria caused a markedly faster progression of the disease than the control bacteria. “The pro-inflammatory bacteria alone only fuel the disease to a limited extent,” explains Anne-Katrin Pröbstel. “But the combination of an inflammatory environment and molecular mimicry activates specific immune cells. These multiply, migrate into the nervous system and attack the myelin sheath there.”
Training the immune system to tolerate rather than attack
The research team conducted the same trials with E. coli bacteria, which are part of the normal intestinal flora and are non-inflammatory. When they implanted the myelin-like E. coli bacteria into the mice, the progression of the disease was milder. “In the future, if we work with different bacteria that actively calm the immune system instead of triggering it, we might be able to train immune cells to tolerate the myelin sheath and not attack it,” says Pröbstel.
The study shows that not only the composition of the intestinal flora plays a role in MS, but that specific myelin-like surface structures on certain bacteria could contribute to the initiation and progression of the disease. It also provides valuable insights into the potential of microbiome-based treatments in MS. These could train the immune system with the help of specifically modified bacteria so that it no longer targets the myelin sheath.
However, the results also call for caution: “Some cancer treatments use the microbiome to stimulate the immune system to combat the tumor,” says Anne-Katrin Pröbstel. “However, this may also create an environment in the intestine in which molecular mimicry can trigger autoimmune reactions or even diseases.”
The study was conducted in collaboration with the University Hospital Bonn, the Cluster of Excellence ImmunoSensation2 at the University of Bonn, the German Center for Neurodegenerative Diseases (DZNE), and other partner institutions. The study received financing from the University Hospital Basel’s Propatient Foundation, the Swiss National Science Foundation and the State Secretariat for Education, Research and Innovation (SERI), among others.
Original publication
Lena K. Siewert, Kristina Berve et al.
Antigen-specific activation of gut immune cells drives autoimmune neuroinflammation
Gut Microbes (2025), doi: 10.1080/19490976.2025.2601430